When Nipples “Point In”: A Specialized Technique for Better Positioning
The Challenge of Nipple Position
Breast reduction surgery is not just about making the breast smaller; it is about reshaping it to look proportional and centering the nipple on the new mound.
Most standard breast reduction techniques (like the popular Superomedial Pedicle) assume the nipple is starting from a standard sagging position. But what happens when a patient’s nipples are naturally positioned medially—meaning they sit closer to the cleavage or "point inward"?
In these cases, using standard techniques can be mechanically difficult. Trying to move an inward-facing nipple into a central position can restrict the blood supply or create tension, limiting how perfect the final result can be.
The Solution: The Superolateral Pedicle (SLP)
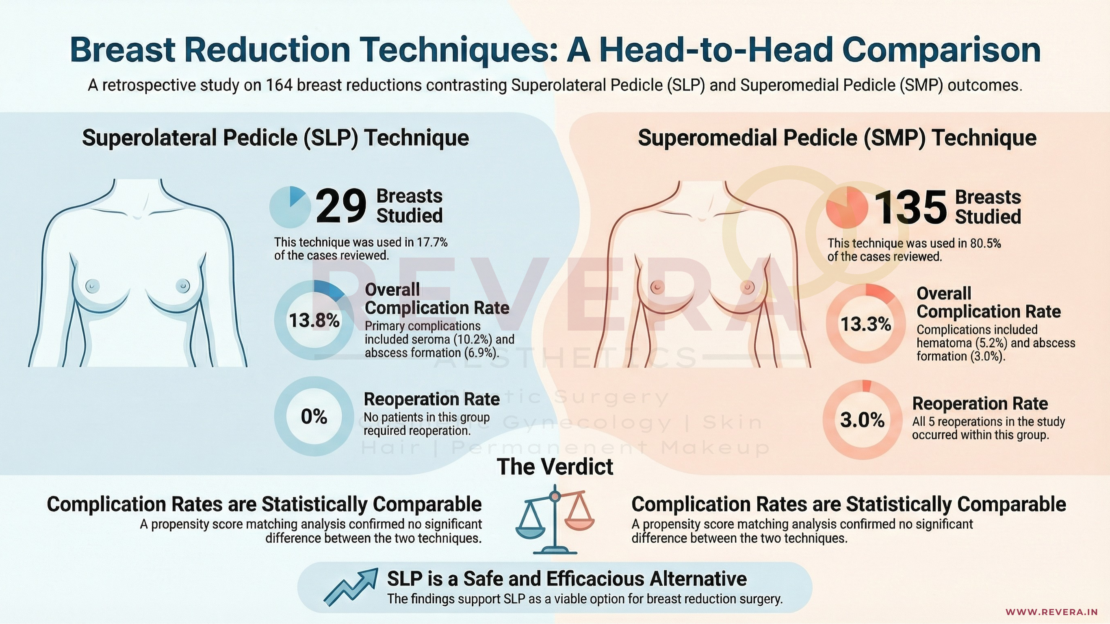
A new study published in Plastic and Reconstructive Surgery (August 2025) highlights a specific surgical approach designed exactly for this anatomy: the Superolateral Pedicle (SLP).
How It Works
In breast reduction, the nipple is kept alive on a "pedicle"—a bridge of tissue that preserves blood vessels and nerves.
- Standard Way (Superomedial): The tissue bridge is usually kept on the inner/top side.
- The SLP Way: For patients with medial nipples, the surgeon keeps the tissue bridge on the outer/top side (Superolateral).
By anchoring the nipple from the outside, the surgeon can more easily swing and rotate the nipple into the perfect central position without fighting the breast's natural tissue resistance.
Is It Safe? The Research Say Yes
Researchers from MedStar Georgetown University Hospital in Washington, DC, reviewed 164 breast reductions to compare the safety of this specialized SLP technique against the standard method.
The Findings:
- Comparable Safety: The complication rates were nearly identical between the two groups (13.8% for SLP vs. 13.3% for standard), proving that this technique is just as safe as the traditional method.
- Effective Reduction: The technique worked well for significant reductions, with an average tissue removal of over 700g.
- No Re-operations: In this specific study group, zero patients in the SLP group required a return to the operating room for complications, compared to 5 cases in the standard group.
Why This Matters For You
Anatomy is unique. If you have noticed that your nipples sit closer to your breastbone or point inward, standard techniques might not offer you the best aesthetic result. This research confirms that your surgeon has a validated, safe "tool in the toolkit" to correct medially positioned nipples and achieve a beautiful, centered look.
Frequently Asked Questions (FAQ)
Q: How do I know if I have "medially positioned" nipples?
A: If your nipples seem to sit closer to your cleavage rather than the center of your breast mound, or if they point inward towards each other, you likely have medial positioning. Your surgeon will assess this during your consultation.
Q: Does this technique leave different scars?
A: generally, no. The Superolateral Pedicle refers to the internal tissue handling. The external scars usually follow the standard "Wise Pattern" (Anchor) or Vertical (Lollipop) shape, just like a regular breast reduction.
Q: Is the recovery harder with this technique?
A: According to the study, complications such as wound healing issues (dehiscence) or fluid collection (seroma) were comparable to the standard technique, suggesting the recovery process is very similar.
Q: Can I still breastfeed with this technique?
A: Like the standard Superomedial technique, the SLP preserves a bridge of tissue carrying blood and nerve supply to the nipple. While breastfeeding can never be guaranteed after reduction surgery, techniques that preserve the pedicle generally offer a better chance than those that do not.
Reference
Lava, Christian X. MS; Li, Karen R. BBA; Episalla, Nicole C. MD; Snee, Isabel A. BS; Bell, Alice C. BA; Fan, Kenneth L. MD; Jabbour, Samer F. MD. "Superolateral Pedicle Breast Reduction for Patients with Medially Positioned Nipple-Areola Complexes." Plastic and Reconstructive Surgery 156(2):p 174e-182e, August 2025.