Awake Breast Reduction: Is General Anesthesia Necessary?
A Revolutionary Approach to Breast Surgery
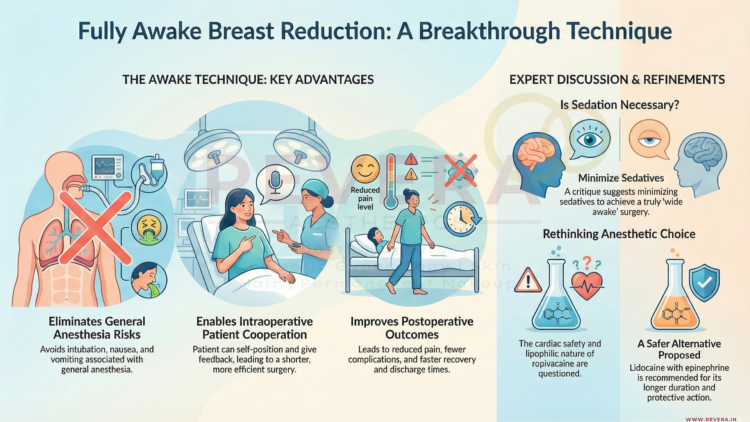
For many women considering breast reduction surgery, the fear is not necessarily of the procedure itself, but of “going under.” General anesthesia, while generally safe, comes with side effects like nausea, grogginess, and a longer recovery time.
However, a study published in Plastic and Reconstructive Surgery presents a compelling alternative: Fully Awake Breast Reduction.
Authors Dr. Simon Filson, Dr. Danielle Yarhi, and Dr. Yitzhak Ramon from Haifa, Israel, successfully performed breast reductions on 25 patients who were awake, communicative, and able to move during the surgery—all without feeling pain.
How Is It Possible?
The secret lies in Thoracic Epidural Anesthesia.
Unlike general anesthesia, which puts the entire body to sleep and requires a breathing tube, a thoracic epidural numbs only the specific area of the body being operated on (the chest). The patient breathes on their own and remains conscious.
The “Awake” Cocktail: Anesthetics and Sedatives Used
To ensure the patient was comfortable, relaxed, and pain-free, the surgical team utilized a specific combination of oral medications and local anesthetics.
According to the study and the accompanying discussion by Dr. Donald Lalonde, the specific protocol included:
1. The “Sedative Cocktail”
Before the procedure began, patients were given these agents to induce relaxation and prevent pain or nausea:
- Oxazepam : A benzodiazepine used to reduce anxiety.
- Dipyrone : A strong analgesic (pain reliever).
- Promethazine : An antihistamine that provides sedation and prevents nausea.
2. The Anesthetic Block (The Numbing Agents)
To perform the epidural block itself, the anesthesiologist used:
- Lidocaine: Injected under the skin to numb the needle entry point.
- Ropivacaine : Injected into the epidural space to provide the actual sensory block for the surgery.
Why Being Awake Changes Everything
The benefits of this technique went far beyond just avoiding general anesthesia. Because the patients were awake, they could actively cooperate during the surgery.
- The “Sit-Up” Test: Patients could sit up on the operating table, allowing the surgeon to check the symmetry and shape of the breasts against gravity in real-time. The patient could even look and give their opinion before the surgery was finished!.
- Faster Recovery: Patients were able to get off the operating table and walk to the recovery room immediately after surgery.
- No “Hangover”: There were zero reports of nausea or vomiting, a common side effect of general anesthesia.
Expert Debate: “Sedated” vs. “Wide Awake”
This technique has sparked interesting conversations among experts. Dr. Donald Lalonde, a Canadian expert in “Wide-Awake Surgery,” applauded the move away from general anesthesia but noted that because sedatives (Oxazepam and Promethazine) were used, the patients were technically “sedated” rather than “wide awake”.
Dr. Lalonde suggested that in the future, surgeons might be able to skip the sedatives entirely and use Lidocaine with Epinephrine for the block, making the procedure truly “wide awake” and eliminating the risks associated with sedatives.
The Future of Surgery
Whether using mild sedation or pure local anesthesia, the trend is clear: surgery is becoming safer, lighter, and more patient-focused. If you are considering breast reduction but fear general anesthesia, this study proves that effective, comfortable alternatives exist.
Reference
- Filson, Simon A. M.B.B.S.; Yarhi, Danielle M.D.; Ramon, Yitzhak M.D. “Fully Awake Breast Reduction.” Plastic and Reconstructive Surgery 138(5):p 978-983, November 2016.
- Lalonde, Donald H. Hon.B.Sc., M.D., M.Sc. “Discussion: Fully Awake Breast Reduction.” Plastic and Reconstructive Surgery 138(5):p 984-985, November 2016.