The New Gold Standard: What the Latest Guidelines (2022) Say About Breast Reduction
Setting the Standard for Safety and Results
Breast reduction surgery (reduction mammaplasty) is one of the most life-changing procedures in plastic surgery, performed on over 100,000 patients annually. To ensure patients receive the safest and most effective care, the American Society of Plastic Surgeons (ASPS) convened a multidisciplinary work group to update their clinical practice guidelines.
Published in 2022, these guidelines reviewed thousands of studies to determine what truly works. Here is what the new evidence means for you as a patient.
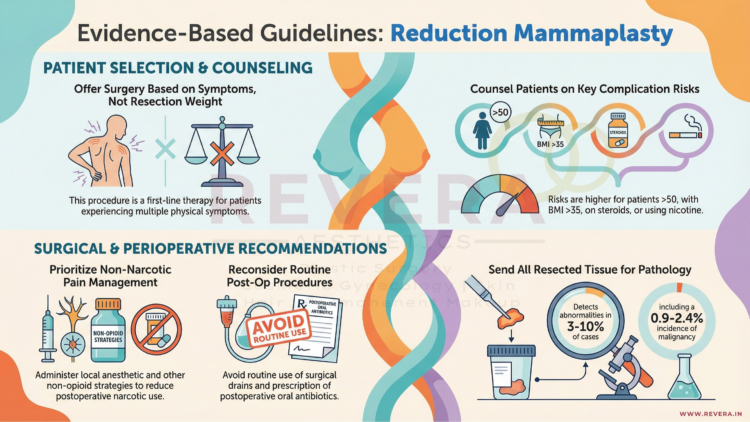
1. It Is About Your Symptoms, Not the Scale
For years, insurance companies often demanded a specific weight of tissue be removed (e.g., 500g or 1000g) to qualify for coverage. The new guidelines challenge this outdated metric.
The ASPS now strongly recommends that surgery be offered as first-line therapy based on symptoms, not resection weight.
- The Evidence: Studies show that relief from back pain, neck pain, and bra strap grooving is not correlated with the amount of tissue removed.
- The Takeaway: If you have multiple physical symptoms (pain, rashes, grooving) that aren’t fixed by non-surgical methods, you are a candidate for surgery, regardless of whether you need a “small” or “large” reduction6666.
2. Drains Are No Longer Routine
One of the most dreaded parts of recovery for many patients is the use of surgical drains (tubes sticking out of the incision to collect fluid).
The guidelines bring good news: Plastic surgeons should not routinely use intraoperative drains for breast reduction patients.
- Why? High-quality evidence shows no significant difference in complication rates (like hematomas) between patients with drains and those without.
- The Benefit: avoiding drains means less discomfort during removal, lower costs, and less scarring.
3. Pain Management Has Evolved (Less Narcotics)
The modern approach to breast reduction focuses on multimodal pain management to reduce the need for strong opioids (narcotics).
- Local Anesthesia: The guidelines strongly recommend administering local anesthetic (numbing medication like lidocaine or bupivacaine) at the surgical site. This significantly improves pain scores immediately after surgery and reduces the time spent in the recovery room.
- Non-Narcotic Strategies: Surgeons are encouraged to use non-opioid medications (such as Acetaminophen or NSAIDs) to manage pain safely.
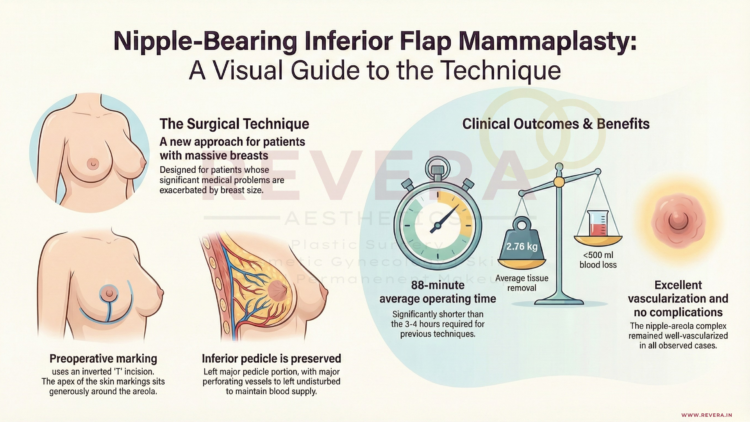
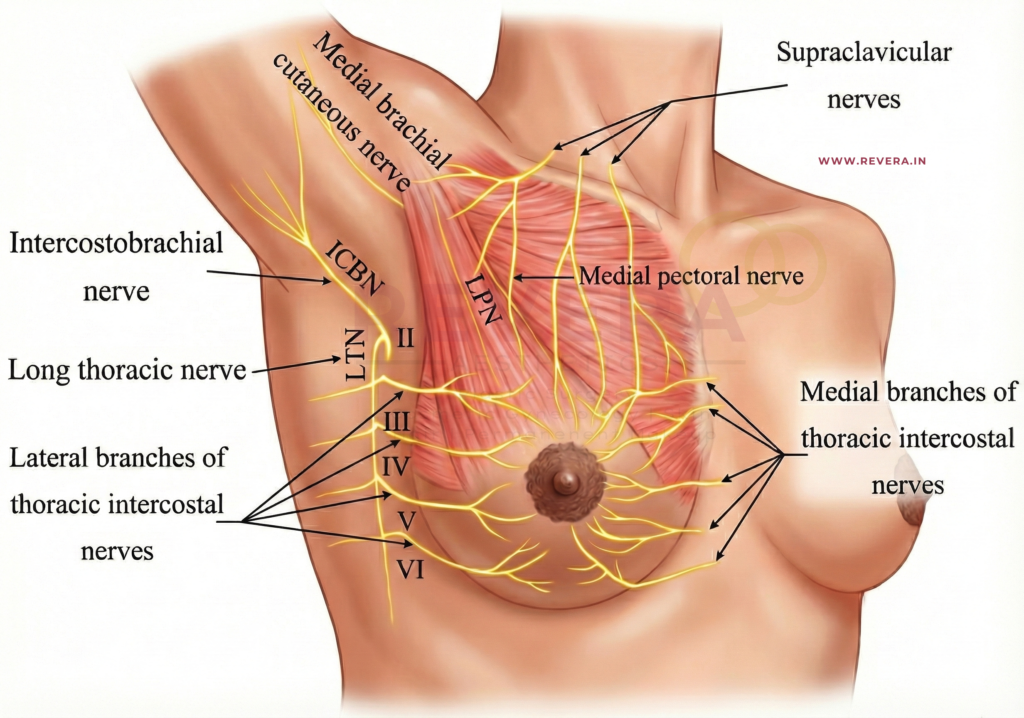
4. Technique: The Pedicle Choice
The “pedicle” is the bridge of tissue that keeps your nipple alive and sensitive during the lift and reduction. The guidelines reviewed the two most common techniques:
- Inferior Pedicle: The most commonly used, reliable for preserving blood supply.
- Superomedial Pedicle: Preserves upper-pole fullness and avoids a long transverse scar.
The verdict? Both techniques are acceptable and effective. There is no significant difference in major complications between them, so your surgeon can choose the method best suited to your specific anatomy.
5. Important Risk Factors
To ensure safety, the guidelines identified specific factors that may increase the risk of complications. Patients should be counseled if they:
- Are older than 50 years.
- Have a Body Mass Index (BMI) greater than 35.
- Use chronic corticosteroids.
Additionally, there is a strong recommendation regarding Nicotine: Patients identified as nicotine users should be referred to cessation programs and encouraged to stop smoking before surgery. Smoking significantly increases the risk of wound healing problems and infection.
6. Antibiotics and Pathology
- Antibiotics: Extended courses of antibiotics after you go home are generally not recommended. A single dose given before surgery (within 1 hour of incision) is sufficient to prevent infection without causing antibiotic resistance.
- Pathology: It is recommended that all breast tissue removed during the surgery be sent to the lab for evaluation to check for any hidden abnormal cells or high-risk lesions.
Frequently Asked Questions (FAQ)
Q: Do I have to try physical therapy before surgery?
A: The guidelines state that reduction mammaplasty should be offered as first-line therapy over non-operative treatments. There is no evidence that non-operative management (like special bras or therapy) provides effective long-term relief for breast hypertrophy.
Q: Will I have drains?
A: According to the 2022 guidelines, routine use of drains is not supported by evidence. However, exceptions may be made for specific high-risk cases or if liposuction is also performed.
Q: Does the “Pedicle” technique affect breastfeeding?
A: The guidelines noted that techniques preserving the subareolar parenchyma (the tissue under the nipple) increase the likelihood of breastfeeding success, but more research is needed to compare specific techniques directly.