Your Post-Breast Reduction Surgery Mammogram: What Has Changed?
The New “Baseline”
If you have a breast reduction, your breasts undergo significant internal changes. It is not just the outside that is reshaped; the internal glandular tissue is moved, stitched, and sometimes combined with liposuction.
Because of this, your mammograms will look different for the rest of your life. Dr. Joan Robertson conducted a study on 50 patients to document these “constant and significant” changes.
Why Does the Image Change?
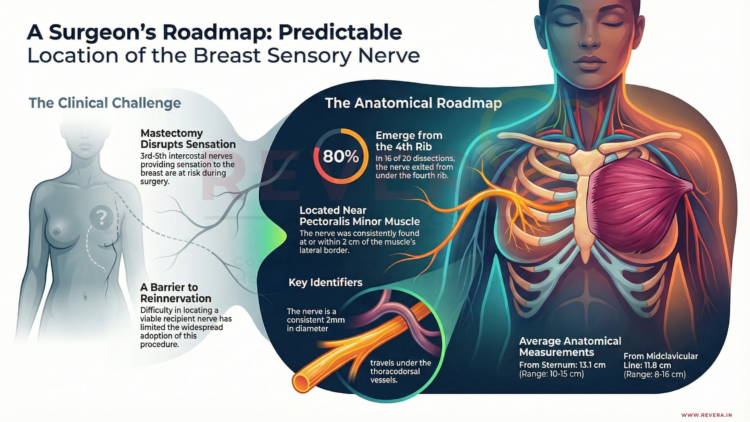
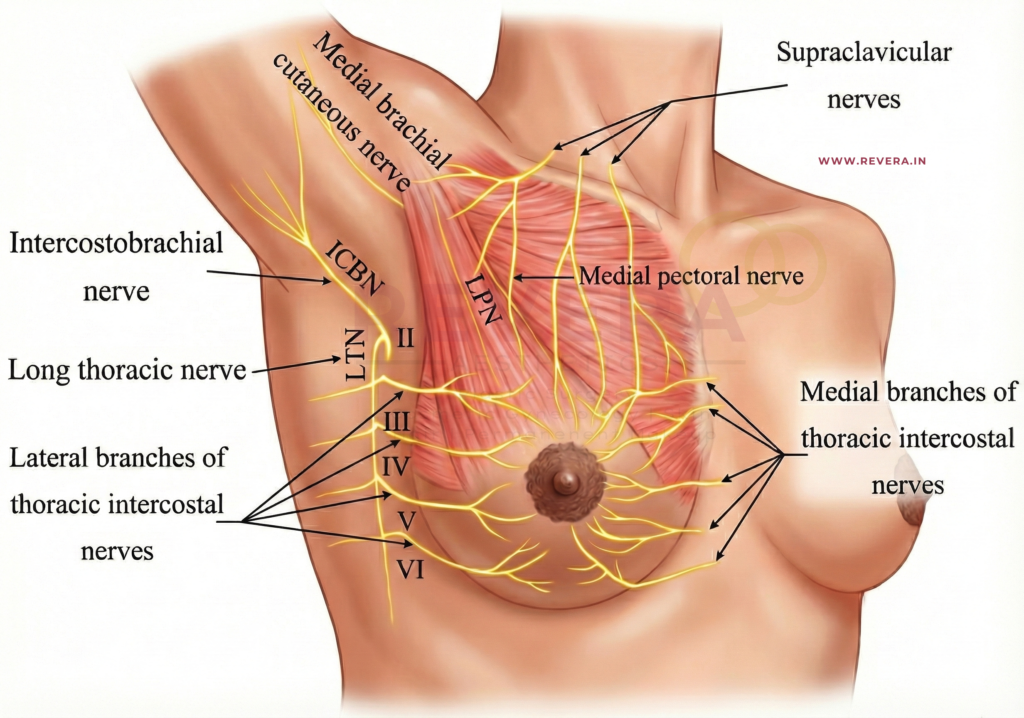
The surgery involves moving the “nipple-areola complex” and the underlying tissue. This shifting creates specific features that a radiologist (a doctor who reads X-rays) must recognize so they don’t mistake them for something more serious.
1. Internal Scarring (Fibrosis)
As the breast heals, internal “scar tissue” forms where the incisions were made. On a mammogram, this can appear as thickened areas or shadows.
2. Oil Cysts and Calcifications
Sometimes, small areas of fat tissue lose their blood supply during surgery. This is called fat necrosis. While harmless, it can turn into “oil cysts” or tiny calcium deposits (calcifications) that show up clearly on an X-ray.
3. The “Mediolateral” Shift
Interestingly, Dr. Robertson found that these changes are often most visible on the mediolateral view (the side-to-side view) rather than the cranio-caudad (top-down) view.
Safety First: The Hidden Findings
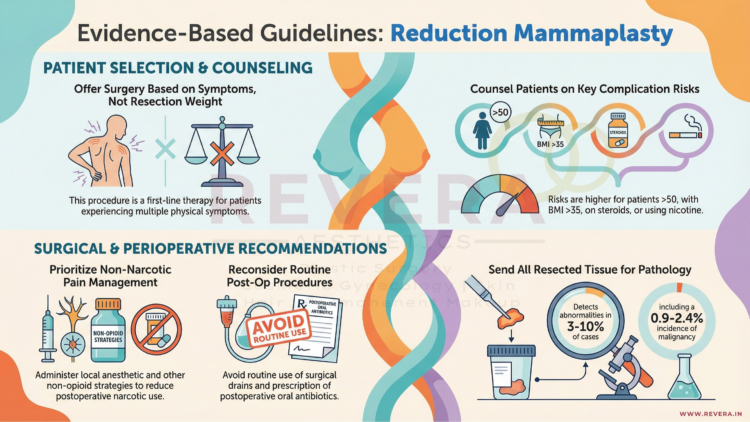
As we discussed in the Emory University study, surgeons always send the removed tissue to a lab to check for hidden abnormalities.
- The Benefit: This routine check catches hidden findings in 1.8% of general patients.
- The Protocol: Having a “normal” mammogram before surgery is standard, but the lab test after surgery is an extra layer of safety.
Tips for Your Future Mammograms
- Wait for the Settling: Most surgeons recommend waiting 3 to 6 months after surgery before getting a new “baseline” mammogram.
- Inform the Tech: Always tell the mammogram technician that you have had a breast reduction. They will place specialized “scar markers” (tiny stickers) on your skin so the radiologist knows where the surgical lines are.
- Provide Old Films: If possible, give your radiologist your mammograms from before the surgery. Comparing the “old” breast to the “new” breast helps them identify which changes are purely surgical.
Conclusion
A breast reduction does not make it harder to detect cancer, but it does change the “landscape” of your breast tissue. By understanding these changes and communicating with your medical team, you can continue your routine screenings with confidence and peace of mind.
Ask yourself “Who is the Best Plastic Surgeon Near Me?”.
Revera Clinic caters with the Best Plastic Surgeon in Hyderabad!
Breast Reduction Surgery Cost varies between individuals!
Contact us to know if you are a suitable candidate for Breast Reduction Surgery!
Frequently Asked Questions (FAQ)
Q: Does breast reduction increase the risk of breast cancer?
A: No. In fact, some studies suggest that because you have less breast tissue after surgery, the overall risk may slightly decrease.
Q: What if my mammogram shows “calcifications”?
A: Post-surgical calcifications are very common. Radiologists can usually tell the difference between “benign” (harmless) surgical calcifications and those that require further testing.
Q: Should I get a mammogram right before my surgery?
A: Yes. The ASPS Guidelines recommend a preoperative mammogram for most women over the age of 35 or those with a family history of breast cancer.
References
- [1] Robertson, Joan L. A. “Changed Appearance of Mammograms Following Breast Reduction.” Plastic and Reconstructive Surgery 59(3):p 347-351, March 1977.
- [2] Razavi, Seyed Amirhossein; et al. “The Incidence of Occult Malignant and High-Risk Pathologic Findings in Breast Reduction Specimens.” Plastic and Reconstructive Surgery 148(4):p 534e-539e, October 2021.
- [3] Perdikis, Galen; et al. “Evidence-Based Clinical Practice Guideline: Revision: Reduction Mammaplasty.” Plastic and Reconstructive Surgery 149(3):p 392e-409e, March 2022.