The “Y-Scar” Technique: Even Less Scarring Than the Lollipop?
The Quest for the Invisible Scar
In the world of breast surgery, the “Vertical” (Lollipop) reduction was a major leap forward because it eliminated the horizontal anchor scar. But for some surgeons, even the circle around the areola was too much.
In December 2007, Dr. David Hidalgo published a study in Plastic and Reconstructive Surgery proposing a radical modification: Deleting the top half of the scar.
He explains Breast Reduction with Minimal Y Scar
This work was done at Weill-Cornell University Medical College in New York.
This paper introduces a refined technique for patients who need a “mini” Breast reduction and want the absolute minimum amount of scarring.
He argued that for certain young patients with mild enlargement, the upper part of the incision is unnecessary and actually harms the aesthetic result.
The Innovation: Saving the Upper Border
The “Y-Scar” technique is essentially a vertical reduction where the surgeon leaves the upper half of the areola completely untouched.
- The Theory: The transition between the darker areola skin and the lighter breast skin is often soft and natural. When you cut through it (as in a standard donut lift), you replace that soft transition with a sharp white scar line.
- The Solution: By leaving the top half of the areola attached to the skin, the surgeon preserves that natural “blur,” making the breast look virtually untouched from the top down. The resulting scar looks like a “Y” (or a lollipop with the top of the circle missing).
Who is the “Y-Scar” Candidate?
This technique is not for everyone. Dr. Hidalgo specifically designed it for a “niche” group of patients who often fall into the gap between a lift and a reduction:
- Mild Macromastia: Patients who only need a small amount of weight removed (the study average was 198 grams, compared to 500g+ for standard reductions).
- Minimal Ptosis: Women with only mild drooping.
- Young Patients: Younger skin has better elasticity, which is crucial for this technique to settle smoothly without bunching.
The Results: High Satisfaction for “Mini” Reductions
The study reviewed 10 patients (8 reductions/lifts and 2 augmentations/lifts).
- Aesthetic Outcome: All patients were pleased with the reduced scar burden. The removal of the upper scar significantly reduced the “perception” of having had surgery.
- Minor Issues: Because the skin is less managed than in full reductions, some patients experienced “inferior fullness” (fullness at the bottom of the areola), but this was considered a minor trade-off for the lack of scarring.
Conclusion
For young women seeking a “perk-up” and a small reduction, the full Lollipop or Anchor scar might feel like overkill. The Y-Scar Vertical Mammaplasty offers a tailored, minimalist approach that respects the natural anatomy of the areola, leaving the upper breast looking completely natural.
Ask yourself “Who is the Best Plastic Surgeon Near Me?”.
Revera Clinic caters with the Best Plastic Surgeon in Hyderabad!
Breast Reduction Surgery Cost varies between individuals!
Contact us to know if you are a suitable candidate for Breast Reduction Surgery!
Frequently Asked Questions (FAQ)
Q: Can this be done if I have very large breasts?
A: Likely not. The study specifically focused on “mild macromastia” (under 400g removal). Larger reductions usually require the full skin tightening power of the Anchor or full Vertical patterns.
Q: Is this different from a “Circumvertical” lift?
A: It is a variation of it. Most vertical lifts cut all the way around the areola. This specific “Y” variation spares the top 180 degrees of the areola rim.
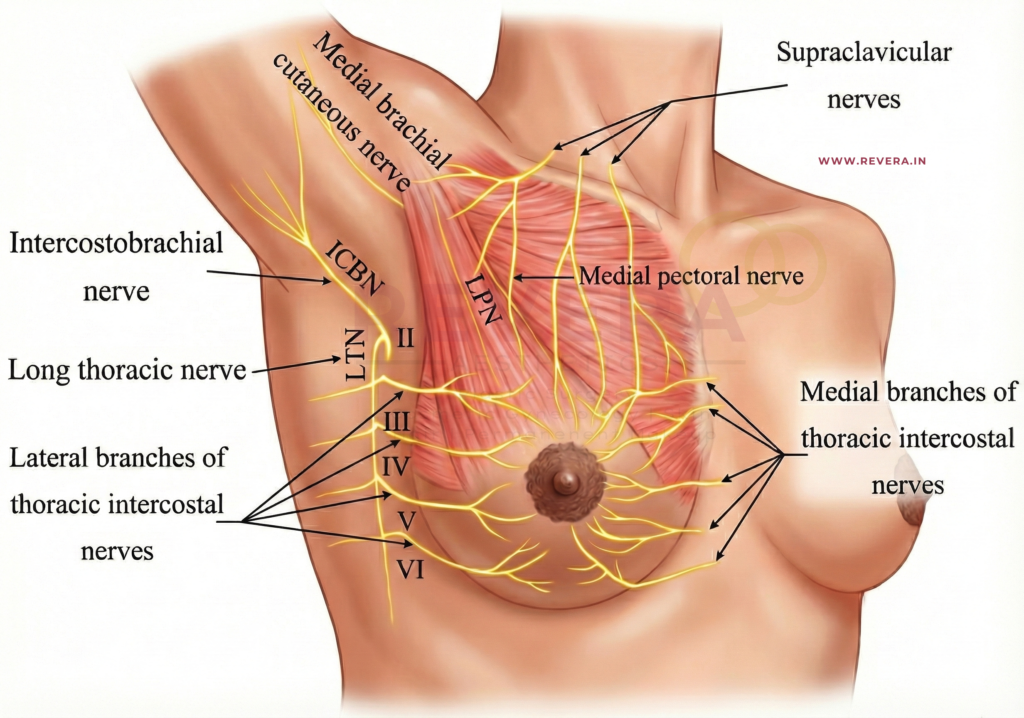
Q: Does it affect nipple sensation?
A: Since the upper skin bridge is left intact, the nerve supply is generally well-preserved, similar to other vertical techniques.
References
- [1] Hidalgo, David A. M.D. “Y-Scar Vertical Mammaplasty.” Plastic and Reconstructive Surgery 120(7):p 1749-1754, December 2007.
- [2] Hammond, Dennis C. M.D. “Short Scar Periareolar-Inferior Pedicle Reduction (SPAIR) Mammaplasty.” Plastic and Reconstructive Surgery, 1999.